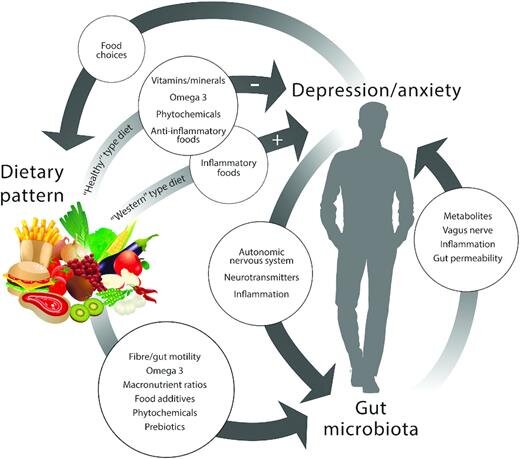
If you have digestive concerns you’re probably well aware that when your digestion is off, your mood suffers as well. And vice versa when mental health is suffering (whether that be excessive stress, low mood, or feelings of anxiety), digestive concerns can flare up. This often results in a vicious cycle. As naturopaths, we use a holistic approach addressing both sides of the equation (mental health and digestion) in order to break this cycle.
Why and how does digestive health impact our mood?
Well first of all, it’s not enjoyable to be in discomfort. But beyond that, there are physiological factors that contribute to the connection between your gut and your mood. The high rates of comorbidity between anxiety and depression and those with inflammatory bowel disease (IBD) or inflammatory bowel syndrome (IBS) have sparked much research into the gut-brain axis. This axis seems to be highly influenced by our gut microbiota.
The bacteria in your digestive tract actually have a way of communicating to your brain by altering your immune system, your nervous system, and your hormones (1). There are a number of suggested ways in which the gut microbiome talks to your brain. A couple propositions include:
Inflammation: different compositions of bacteria in the gut can either result in increased or decreased inflammatory mediators that directly affect brain function (1). The vagus nerve, which is responsible for our “rest and digest” nervous system also maintains anti-inflammatory capacity. Many of the effects of the microbiome seem to be dependent on vagus nerve function (1). Furthermore, bacteria that produce more inflammatory compounds seem to be increased in those with depressive episodes (2).
Neurotransmitter production: many bacteria actually produce neurotransmitters which are the signalling molecules in our nervous system. Lactobacillus and Bifidobacterium species produce GABA; Candida, Streptococcus, Escherichia, and Enterococcus species produce serotonin; and Bacillus species produce dopamine (1). However, understanding how these microbial-produced neurotransmitters affect our central nervous system is still a work in progress.
Dysbiosis: an imbalance of the microbiome
The type, amount, and location of bacteria are important in keeping a healthy, balanced digestive system and therefore gut-brain axis. A variety of bacteria is important for a balanced microbiome, but as we saw previously some bacteria are more helpful than others. In mood disorders we see that the diversity and composition of the gut microbiome is altered (2).
The amount of bacteria and where they hang out in your digestive tract also contribute to the balance. The large intestine harbours the greatest numbers of bacteria (in the trillions) with the small intestine typically carrying much smaller amounts (in the millions). However, an overgrowth of certain bacteria in the small intestine occurs in over a third of those people diagnosed with IBS (3). This is called small intestinal bacterial overgrowth (or SIBO) and is one of the more common forms of dysbiosis.
Symptoms of a dysbiosis:
Bloating: often worse with certain foods that trigger unwanted bacteria (wheat, garlic, onion, beans, legumes)
Abdominal pain or discomfort
Changes in bowel movements: constipation, loose stools, or diarrhea
Mood alterations
Balancing your gut microbiome
Eradication of unwanted bacteria: using natural or pharmaceutical antimicrobials
Repopulation of good bacteria: using targeted types of probiotics. Ingestion of probiotics has actually been shown to reduce anxiety symptoms (4).
Maintaining optimal digestive processes: by promoting stomach acid production and gastrointestinal motility.
Nourishing good bacteria: using healthy diet and prebiotic foods such as fiber. See the diagram below for details on how diet, microbiome, and mental health are all linked (5).
To book an appointment with a Naturopath at Juniper Family Health, please contact the clinic at 778-265-8340 or info@juniperfamilyhealth.com or click here to book online.
References:
Cryan, J., Dinan, T. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nature Reviews, 13, 701-712.
Huang, T., Lai, J., Du, Y., Xu, Y., Ruan, L., Hu, S. (2019). Current understanding of gut microbiota in mood disorders: an update of human studies. Frontiers in Genetics, 10, 98.
Mann, N., Limoges-Gonzales, M. (2009). The prevalence of small intestinal bacteria vergrowth in irritable bowel syndrome. Hepato-gastroenterology, 56(91-92), 718-721.
Ding, H. (2018). Gut microbiota and anxiety: an exploration of key findings. Journal of Anxiety and Depression, 7, 1.
Bear, T., Dalziel, J., Coad, J., Roy, N., Butts, C., Gopal, P. (2020). The role of the gut microbiota in dietary interventions for depression and anxiety. Advances in Nutrition, 1-18.